POSTED : September 20, 2022
BY : Stephanie Cohen

In our whitepaper, Loyalty in Healthcare: Creating Connected Membership, we discussed how in a time of increasing consumerism and industry disruption, both payers and providers need to create stronger relationships with their members and patients. We reviewed this task through the lens of loyalty, focusing on creating strategies to increase the value associated with these relationships, through establishing deliberate and curated journeys that resonate with target audiences.
But, connected membership is not only an option for consumers—it can also apply to how a health plan (aka plan, payer, insurer) interacts with its providers (i.e., hospitals, clinics, physicians, nurse practitioners, physicians’ assistants, therapists, nutritionists, etc.).
Traditionally, payers create networks of healthcare providers to provide care to their members. The payer wants to ensure that its members have adequate coverage and reasonable choices to meet their needs, while managing the cost of care. So, the networks need to balance quantity, quality, and cost to assure optimal results.
Although some providers may choose not to affiliate with payers, most find value in being part of at least one network, so that they can have support getting patients, and get paid for taking care of those patients. Insured individuals want to stay in network, so they can get coverage for their health, receive generally lower negotiated rates, and avoid having to pay more than their deductible or copay up front. Members also receive some level of confirmation that the in-network provider has met at least the minimal standards for care. It’s a win-win.
To become part of a payer network, providers need to be credentialed first by the payer (which can be a lengthy frustrating process) and then go through contracting. There is a lot of paperwork over an extended period of time, and with at least the smaller practices, the payer holds the upper hand. Once that is finished, then the provider then becomes part of the network. Providers who seek payers as a major patient acquisition and revenue stream contract with multiple payers if practicing in an area covered by multiple plans. Credentialling and contracting with commercial payers can average 90-120 days. A provider is not considered in-network until that process is complete.
The relationship between the payer and the provider is not a seamless one. Providers complain about health decisions being overridden by the plan, ambiguous and changing medical necessity clauses, time-consuming prior authorization processes, payment delays, paperwork to support payment, and inadequate support (tools, longitudinal data, and startup investment) to execute the complex mechanics of value-based contracts, to name a few. Although this may be overstating it a bit, the relationship is often an adversarial one versus one in which both provider and plan collaborate with each other to improve healthcare access and health outcomes for their shared customers.
To better understand the situation, we met with a wide range of providers, from small orthopedic practices to surgical centers to major hospital and dental providers. The pain points were consistent across the provider landscape.
For example, the process by which providers need to obtain authorization for payment is manual and time-consuming. It’s no surprise that providers don’t have the staff to sit on the phone on hold and wait for a response. This puts an enormous burden on their staff, particularly in these times of staffing shortages.
Authorization denials are especially frustrating, especially at the end of the year when patients need essential care. When denials happen, the only course of action is a peer-to-peer review. Often the “peer” is not necessarily a “peer.” This only exacerbates the frustration of the provider.
It’s obvious that reimbursement has been the biggest strain on the payer/provider relationship, but even that can be improved with a provider-centric approach to negotiations.
We believe that the provider-payer relationship can, and should, change. Payers and providers are two sides of the same “patient experience and loyalty” coin, especially when the driving tenet of the value-based care model is one of delivering better value (or health outcomes) for every healthcare dollar spent by a patient.
Providers are both important payer partners and payer customers. Providers can also serve as an important source of goodwill and positive word of mouth to both their patients and other providers.
So how do we believe payers can better foster these relationships? By rethinking and recentering how they engage with providers. Some of what we discuss below may already be in play at some payers, but even if it is, it’s a set of one-off tactics versus a holistic strategy. This is especially relevant as payers would like to see more of their provider networks adopt value-based care and associated reimbursement models that shift more of the risk to providers, and away from themselves. They need to better recognize the value that each party brings to the table and how that can be facilitated.
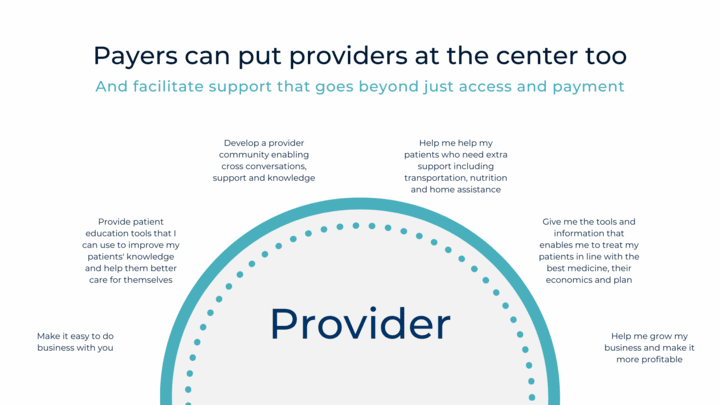
Here is a sample of six broad categories that can build and sustain stronger relationships. You will note that they are written in a provider’s voice, as it is important that any strategy is provider-centric, reflecting their needs and interests. Each category listed above is supported by tactics that may already be in place, but potentially could be improved or even positioned more appropriately.
Make it easy to do business with you. Providers want to focus on treating patients, not fighting with insurance companies. So, payers should look at all their processes through a provider lens and assess where improvements in experience would be beneficial. This can start with the credentialling and contracting process, but extend to other areas such as payments, questions, prior authorizations, and transparent information sharing. For example, research by the Council for Affordable, Quality Healthcare (CAQH) reveals there are significant administrative costs associated with manual prior authorizations for both payers ($3.50 for each transaction) and providers ($6.61 for the same transaction). Going electronic can bring that down to $2.80 per transaction for payers and $0.03 for providers.¹
Help me grow my business and make it more profitable. Providers are also running a business and want to ensure that that business is viable. Payers can identify ways in which they can help support the provider’s success. This can include member-engaging “doc find” tools that include accurate and up-to-date information to help drive new patients to providers. But, it can also include payment efficiencies, collection support, and other functional assists. Depending on the type of provider, the region, the regulations, and perhaps even the demographics and needs of the patients, the payer can develop unique support that bolsters the provider’s practice and creates a stronger relationship.
Give me the tools and information that enables me to treat my patients in line with the best medicine, their economics and their plan. Providers want to provide care and support their patients so that they have the best health outcomes. Easily understanding the individual’s plan eligibility and benefit information, as well as longitudinal health history, may not only help the patient improve compliance, but can also improve their experience and loyalty to the plan and provider, as it relates to recommending a treatment plan that aligns with a patient’s overall health and finances. For example, knowing if a medication is in formulary, and what the expected price is, and how much is paid for by the plan versus by the patient can help guide a provider’s prescribing. If there is an alternative that provides the same prescriptive support, but is more affordable, the provider may choose that drug. This avoids the patient going to the pharmacy, discovering that the price is too high, and then having to contact the provider for a different medication or forgoing it entirely, which has a significant impact on both costs and health outcomes.²
Help me help my patients who need extra support, including transportation, nutrition, and home assistance. As we know, much of an individual’s health and wellbeing are determined by their zip code and not from their genetics. People struggle with food insecurity, unsafe living conditions, and limited access to transportation. Providers may be better able to treat the illnesses that patients have if the patient can get to the office for appointments, have access to digital media for telemedicine support, funds for prescriptions and/or access to healthy foods. As payers and providers address social determinants of health, they should recognize that there is value in creating a partnership with each other (and the individual) that will help improve outcomes.
Provide patient education tools that I can use to improve my patients’ knowledge and help them better care for themselves. Patients often self-diagnose, using “Dr. Google.” And whereas, admittedly, there are legitimate sources of information on the internet being posted by reputable organizations, the guidance given may contradict or be totally erroneous to the patient’s situation. If payers and providers worked together to establish relevant content that the provider could recommend, then not only does it support a patient’s wellbeing, but it also creates incremental connections between the provider, the payer, and the patient.
Develop a provider community enabling cross-conversations, support, and knowledge. The path to sustainability and improved health outcomes requires a collaborative effort. Collaboration fails when there is no trust or alignment to shared objectives among parties. Access to communities of shared interest can improve connectivity and engagement, thus building more trust and alignment. Establishing that type of mechanism can enable three-way conversations: payer to provider, provider to payer, and provider to provider. This can support discussions on health topics, insurance-related topics, and professional guidance, among other things. It can be a space where conversations can be fluid and helpful, and stronger connections can be formed.
This desire for better collaboration is continually echoed by providers across all disciplines in the same way: “Help us help our patients. It’s that simple and that complex at the same time.” They understand it takes a village to bend the curve and improve the health of shared customers while reducing healthcare cost, and they are willing to partner with payers that are willing to work collaboratively with them.
These suggested improvements serve as a microcosm of how payers can rethink their relationships with providers and in doing so, improve not only their stickiness with patients, but their patients’ health and wellbeing as well—the shared end goal for all three parties. Members/patients as healthcare consumers value brands that enable them to engage seamlessly, where they perceive they are valued, and where the brand recognizes their needs and interests and caters to them. Payers and providers can meet the needs of their shared customers when they work together to do so. This approach creates brand differentiation, potential cost savings (both directly with providers, but also indirectly through improved patient outcomes), and positive word of mouth. By putting providers in the center, and regarding them as valued partners, the opportunity exists to change the narrative, ultimately satisfying the expectations of all parties and improving patient health outcomes.
Discover more about how Catalyst supports both payers and providers.
¹ “The CAQH Index Report,” Council for Affordable, Quality Healthcare (CAQH), 2021.
² “Medication Non-Adherence: A Proactive Approach to Reducing Risk,” LexisNexis Risk Solutions, 2022.

Senior Principal, Integrated Loyalty Solutions

VP, Strategic Accounts

VP, Healthcare Solutions

Principal, Design